CU Nursing-led pilot project boosting mental health care in local clinics
Debra Melani | College of Nursing Dec 26, 2019
Patients with substance-use or other mental health disorders at CU Nursing’s Sheridan Health Services clinics are bucking a national trend: They’re getting professional help.
While mental health issues strike one out of five U.S. adults each year, only half of those who seek treatment ever follow through on psychiatric referrals.
“The rest are being seen by primary care providers (PCP),” said Sarah Stalder, a psychiatric mental health nurse practitioner with the University of Colorado College of Nursing.
“Not only do some of those patients need more expert care, but that’s a huge burden on those providers, who often have limited time with patients,” Stalder said.
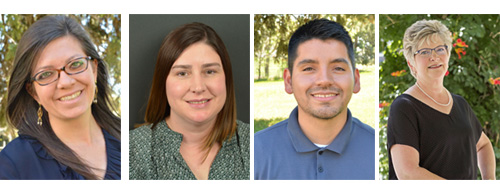
She and her team, led by CU Nursing Professor Amy Barton, PhD, are conducting a pilot project at the Sheridan adult and youth clinics focused on using a collaborative care model to help reverse this sometimes-deadly trend.
Project targets new mental health crisis solutions
“Colorado is ranked ninth among states for age-adjusted deaths due to intentional self-harm,” Barton said, referring to one potential end-result of serious mental issues left untreated. “So obviously, we need new solutions in order to address this crisis.”
Barton and some of her team members shared highlights of their work during the December Nursing Grand Rounds.
By combining a team of PCPs, care coordinators, case managers, and mental health experts in one location, collaborative care allows for an array of services aimed at boosting treatment in an efficient setting.
The already nurse-led, inter-professional environment at Sheridan Health Services clinics provides an ideal setting for the model, a partnership with primary care providers that moves beyond other integrated care models.
More than 80 randomized controlled trials worldwide support collaborative care in primary care settings, Stalder said. The Sheridan project, funded by the Health Resources and Services Administration (HRSA), is now in its fourth year.
Project improves care, tackles hurdles to access
Studies repeatedly show that the model, which largely addresses hurdles to care, boosts access and improves outcomes, Stalder said. The Sheridan project’s results mirror those findings.
Baseline scores in participants with depression improved 41% within two years of the program’s launch. For patients with bipolar disorder, scores rose by 50%.
A four-tiered system unique to the model helps address a national shortage of trained mental health care providers by treating all patients more efficiently and achieving remission of symptoms sooner. In the United States, 60 percent of counties have no practicing psychiatrist.
After assessment, providers place patients into a tier, with monitoring of outcome measures integral to the collaborative care model:
- Mild cases with little safety risk stay with the primary care provider for treatment, as long as the patients continue progressing toward remission of symptoms.
- Moderate cases with slightly more safety risk see their PCP, who consults regularly with a mental health care professional.
- Higher risk patients see both a PCP and a mental health expert concurrently. The providers work as a team.
- Serious cases, generally with psychoses, are referred out for more intensive treatment than the clinic can provide.
Having both physical and mental health care providers working together in one setting helps reduce patient dropout from therapy and psychiatric services.
“We’ve thought of physical and mental health care as separate for a long time. This combines them.”
Collaborative care: treating ‘one person with one team’
A population-based registry and tracker system also plays a chief role with compliance, said Carlo Caballero, LPC, the team’s case manager. Caballero monitors the computerized registry and serves as a patient advocate.
“I really focus on assessing patients’ needs, connecting them with internal and external resources, scheduling appointments for patients, and bridging the gap between patient and provider,” Caballero said. “Basically, it’s being a guide for patients throughout their treatments so they don’t get lost.”
Many issues can lead to healthcare access problems, including homelessness and lack of transportation, which burden the clinics’ largely underserved population.
Taxi vouchers, food banks and low-income housing are types of resource referrals he makes to prevent treatment dropout, Caballero said.
PCPs and mental health experts working in tandem also helps with patient screening and accurate diagnoses, Stalder said. Some physical symptoms can mimic mental health disorders and vice-versa, she said. Moreover, many physical ailments come with mental health symptoms, such as heart disease and depression.
“We’ve thought of physical and mental health care as separate for a long time,” Stalder said. “This combines them. We are treating them as one person with one team, and that’s the way it should be,” she said.
“The biggest thing is reaching the right people with the right treatment at the right time,” Stalder said. “And I think that’s what collaborative care helps us do.”